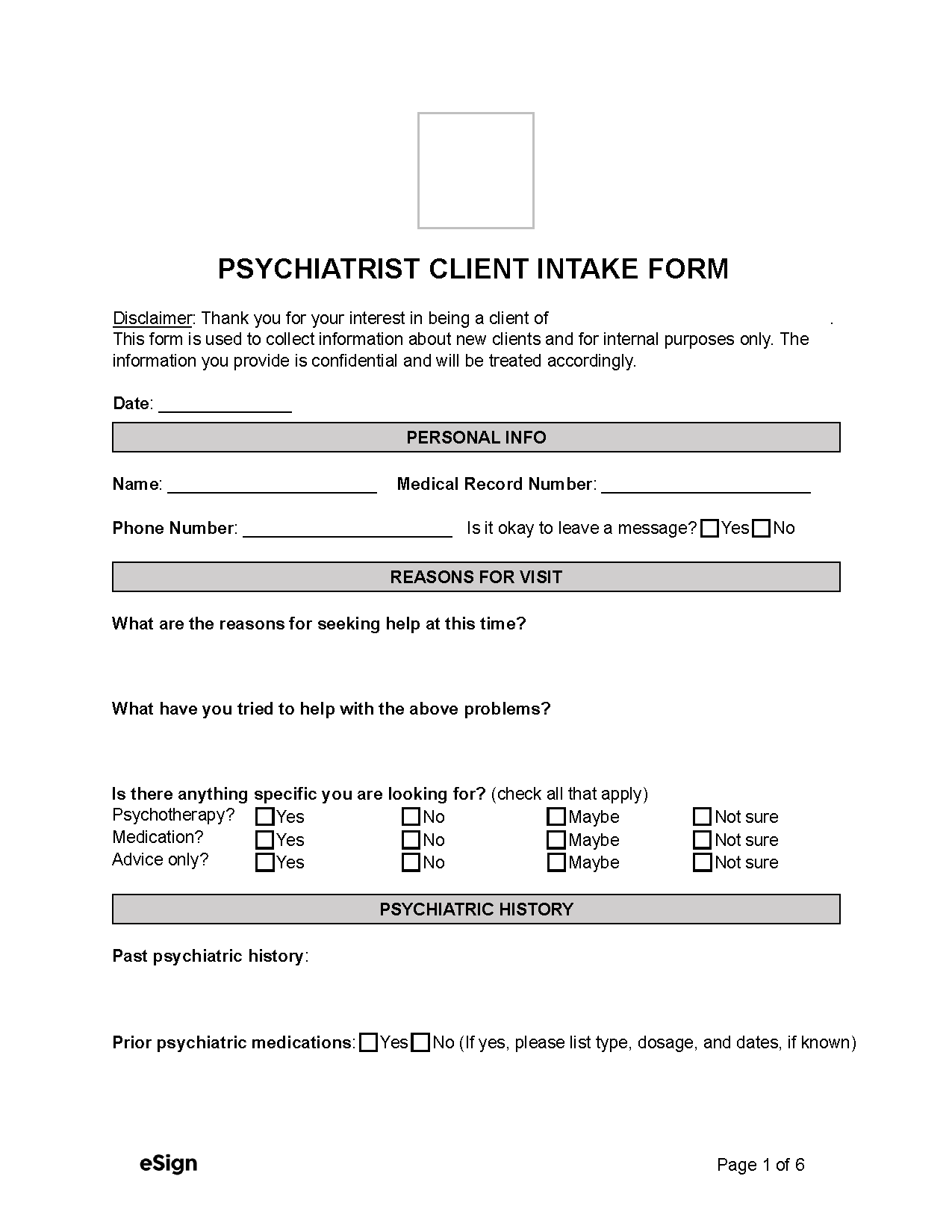
Form Overview
1. Personal Info – The patient should provide their name and contact information.
2. Reasons for Visit – This section asks the patient about the issues they are facing, anything they’ve done to remedy the problem, and what kind of assistance they seek (e.g., therapy, medication, advice, etc.)
3. Psychiatric History – The patient must specify any history of mental illness diagnoses or treatments and if they’ve taken psychiatric medication or received psychiatric hospitalization.
4. Psychological Assessment – The psychological assessment is used to examine the following aspects:
- The patient’s current mental and emotional state
- How various situations affect them
- Any symptoms of trauma, suicidal thoughts, or other mental health issues
- Their habits, behavior, and personality
5. Alcohol or Other Drug Use – The patient will need to describe their current and past alcohol and drug use, specifying how frequently they drink and whether they believe they have an alcohol or drug problem.
6. Personal/Family Data – The patient’s details, such as marital status, education, profession, and ethnicity, should be provided. The form will also gather information about the patient’s family, including any history of mental illness and whether they live with the patient.
Confidentiality and Patient Intake Forms
The HIPPA is a federal law that prevents health professionals, including mental health professionals, from disclosing certain health information unless the patient gives consent.
Similarly, the Substance Abuse and Mental Health Services Administration has established confidentiality regulations that further protect the privacy of a patient’s substance abuse treatment records. However, it’s important to note that clinics and professionals may be required to disclose protected information in emergencies to ensure the safety of the patient or others.