Age of Consent for Treatment
Many states have a minimum age of consent for clients who wish to receive treatment. If a client is under their state’s age of consent, they will require their parent or guardian’s approval, except in emergencies or special situations.
Form Contents
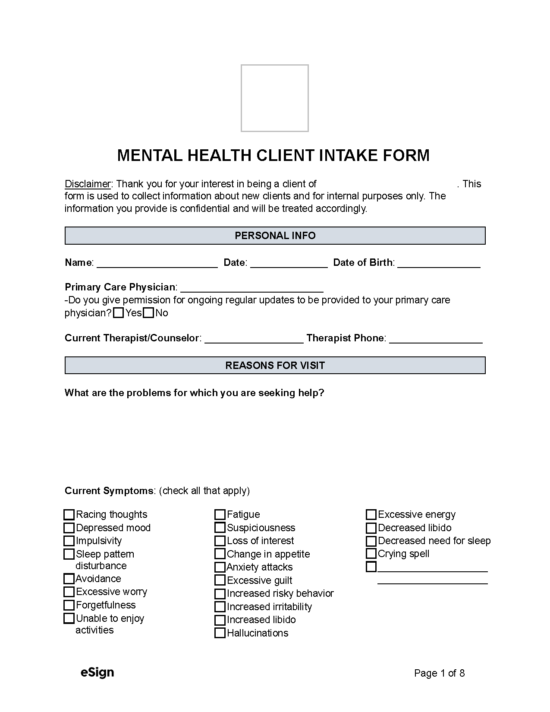
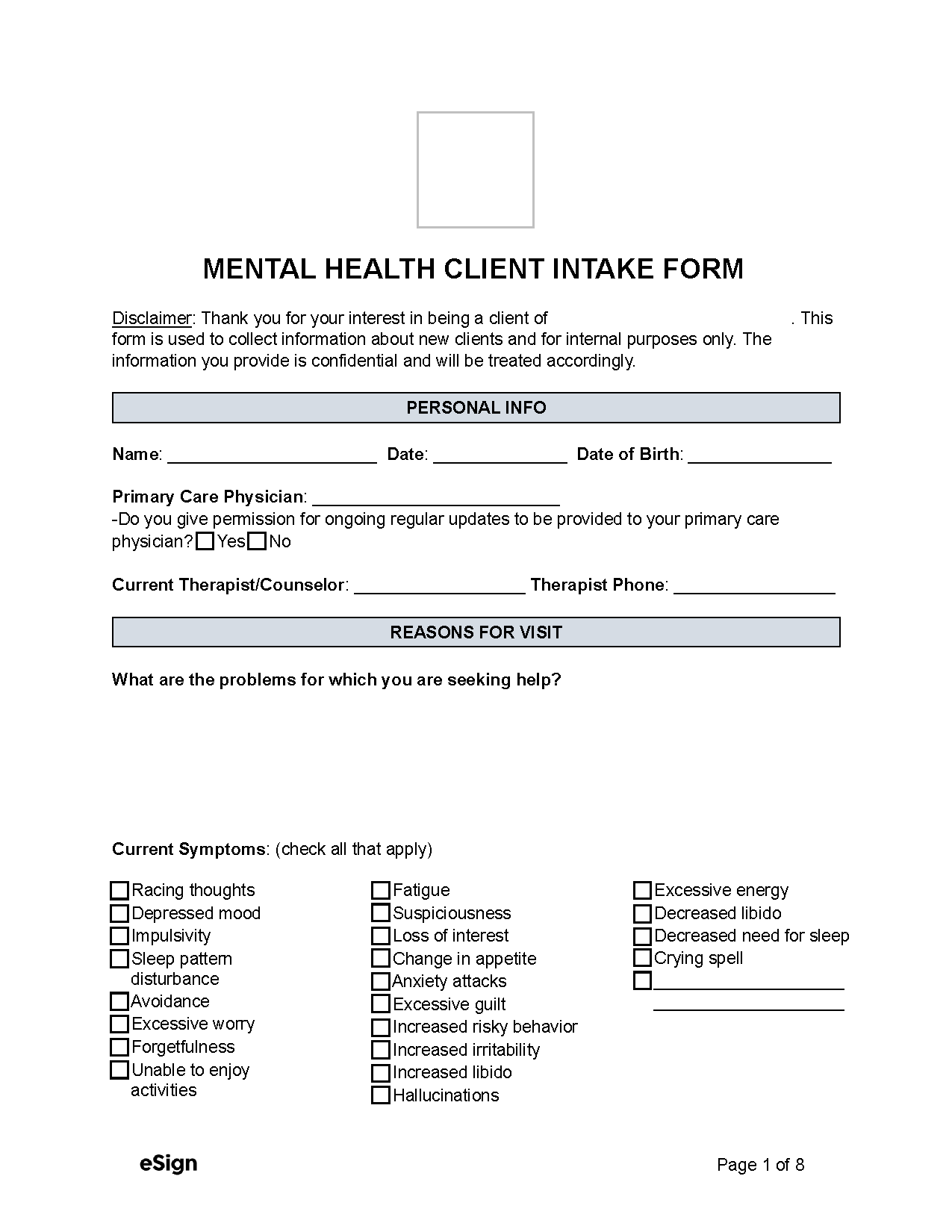
- Personal info – The client’s name, date of birth, address, and current therapist or counselor’s name and phone number.
- Reasons for visit – The client’s issues, symptoms, and assessment of the risk of suicide.
- Medical history – Any allergies the client has, medication they are taking, and current or past medical problems.
- Personal and family medical history – Specifies if the client or any family member has medical problems.
- Psychiatric history – Details any outpatient treatment received, psychiatric hospitalization, and psychiatric medication they are taking.
- Family psychiatric history – The client must state whether anyone in their family has been treated for a mental illness or disorder and whether they’ve been treated with psychiatric medication.
- Personal habits – Details the client’s lifestyle habits and their history with alcohol and drugs.
- Personal details – Outlines details regarding the client’s family, upbringing, history of abuse, and marital, employment, and education information.
- Acknowledgment – The client’s signature and signing date, and, if required, their guardian’s signature.
Informed Consent for Mental Health Treatment
Informed consent occurs when a mental health professional explains the treatment to their client, including risks, benefits, and other options so that the client can make an informed decision. Professionals are legally required to obtain their client’s informed consent before treatment, although the specifics vary from state to state.
Some states also require mental health professionals to provide certain disclosures before beginning treatment.
Health Insurance Portability and Accountability Act (HIPAA)
Under the HIPAA, a client’s information, including information collected electronically, must remain confidential and can only be disclosed with their consent or when required for treatment, payment, or healthcare activities.
Client details may also be disclosed in emergencies, such as when they pose an immediate threat to themselves or others.