Minors in Therapy
The age of consent for therapy varies from state to state.[1] Generally, patients must be at least 18 years old to consent to therapy, though exceptions are made for substance abuse treatment, minors in dangerous situations, and those serving in the military.
Some states allow minors aged 12 or older to consent to therapy, provided their parents are notified, unless doing so would be adverse to the minor’s well-being.
Therapist Confidentiality
The privacy of client information is protected by state and federal laws, including the HIPAA (Health Insurance Portability and Accountability Act).[2] Furthermore, psychotherapy notes are given special protection under the HIPAA and are not subject to the same exceptions as other medical info (i.e., disclosure for treatment, payment, health care operations).[3]
That said, clinics may disclose confidential patient information if the patient consents, if required by law enforcement, or to prevent an immediate threat to the patient or others.
Sample
Download: PDF, Word (.docx), OpenDocument
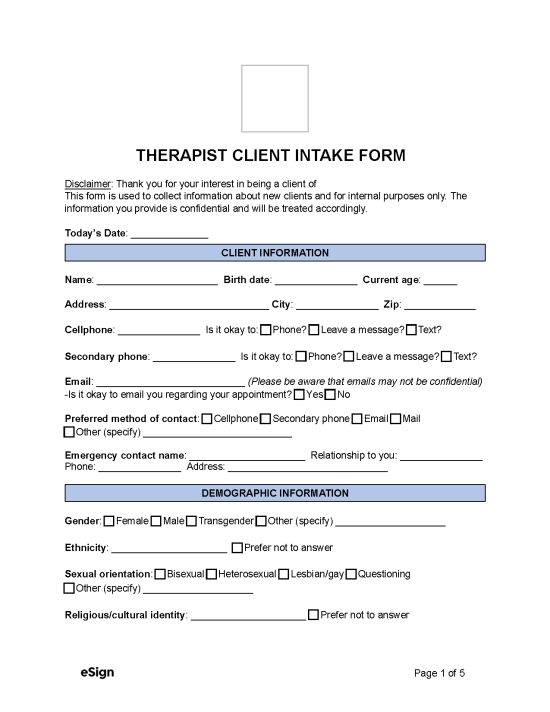
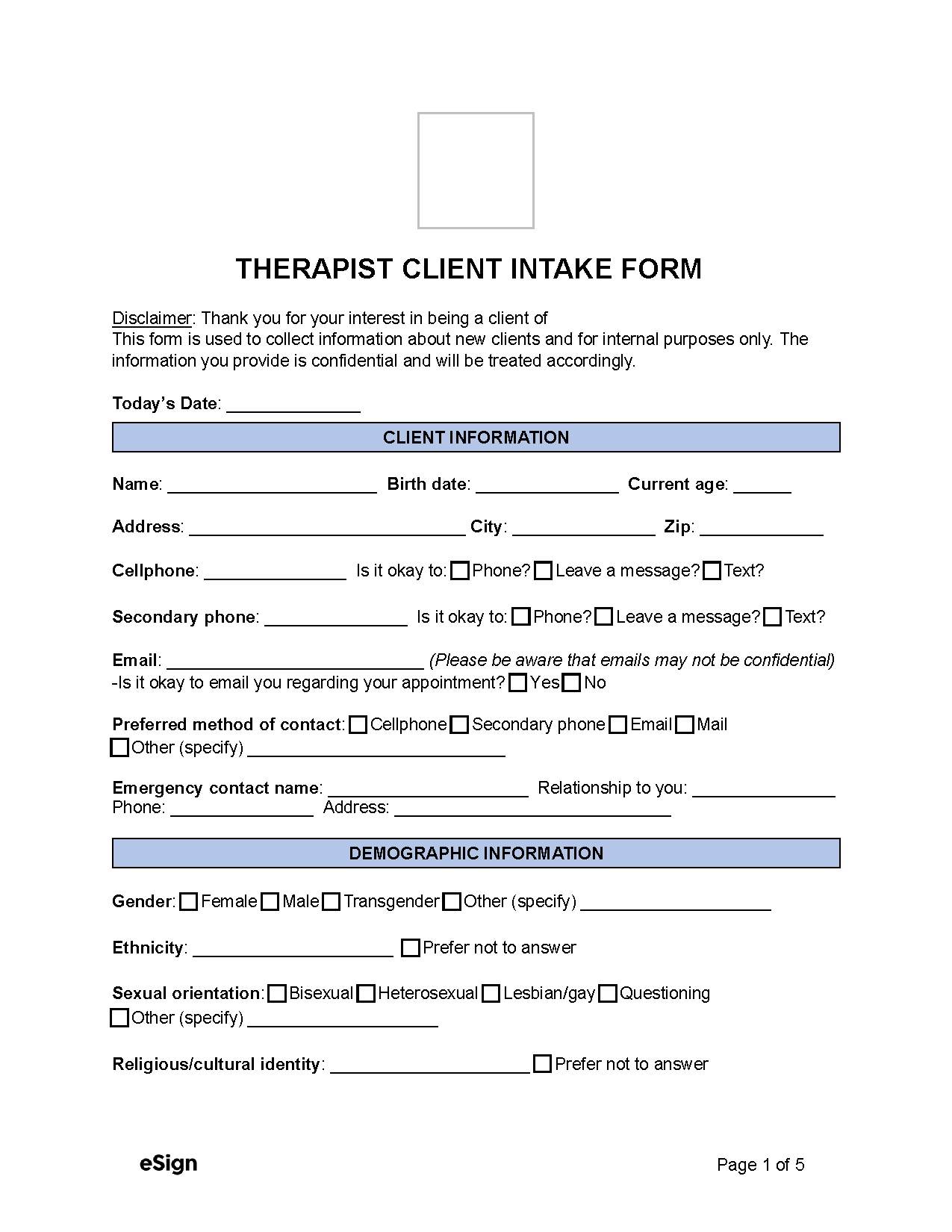
THERAPIST CLIENT INTAKE FORM
DISCLAIMER: Thank you for your interest in being a client of [CLINIC NAME]. This form is used to collect information about new clients and used for internal purposes only. The information you provide is confidential and will be treated accordingly.
CLIENT INFORMATION
Name: __________________ Birth Date: _______ Address: ____________________
Phone: ____________________ Is it okay to: ☐ Phone? ☐ Leave a message? ☐ Text?
Email: ___________________________ (Emails may not be confidential)
DEMOGRAPHIC INFORMATION
Gender: ☐ Female ☐ Male ☐ Transgender ☐ Other (specify) ____________________
Ethnicity: _____________________ ☐ Prefer not to answer
Sexual orientation: ☐ Bisexual ☐ Heterosexual ☐ Lesbian/gay ☐ Other
Relationship status: ☐ Single ☐ Partnered ☐ Married ☐ Separated ☐ Divorced
☐ Widowed ☐ Other (specify) ___________
Check the highest degree you’ve earned: ☐ GED ☐ High school
☐ Associate’s degree ☐ Bachelor’s degree ☐ Master’s degree ☐ Doctoral degree
HEALTH HISTORY
Primary care physician name: ______________________________
How is your physical health? ☐ Poor ☐ Unsatisfactory ☐ Satisfactory ☐ Excellent
Do you take medications, over-the-counter drugs, or supplements? ☐ Yes ☐ No
Have you ever been assessed for psychological or learning issues? ☐ Yes ☐ No
-If yes, please explain, including when and by whom, and the findings/diagnosis:
____________________________________________________________
Have you been prescribed psychiatric medication in the past? ☐ Yes ☐ No
-If yes, please list what medications, the dosage, and when taken:
____________________________________________________________
Have you ever been hospitalized for psychiatric reasons? ☐ Yes ☐ No
FAMILY AND SOCIAL INFORMATION
List the family members to whom you are close:
____________________________________________________________
Any family history of mental illness, substance abuse, or learning difficulties? ☐ Yes ☐ No
PRESENTING CONCERNS
Briefly describe what brings you to this clinic:
____________________________________________________________
Approximately how long have these concerns been bothering you?
☐ A week ☐ A month ☐ Few months ☐ A year ☐ Few years ☐ Most of my life
How much do these concerns interfere with your:
Daily routine: Very little – ☐ 1 ☐ 2 ☐ 3 ☐ 4 ☐ 5 – Severely
Emotional well-being: Very little – ☐ 1 ☐ 2 ☐ 3 ☐ 4 ☐ 5 – Severely
Relationships/activities: Very little – ☐ 1 ☐ 2 ☐ 3 ☐ 4 ☐ 5 – Severely
ACKNOWLEDGEMENT
Signature: _________________________ Date: ___________
Printed Name: ____________________
Guardian Signature (if required): ________________________ Date: ___________
Printed Name: ____________________