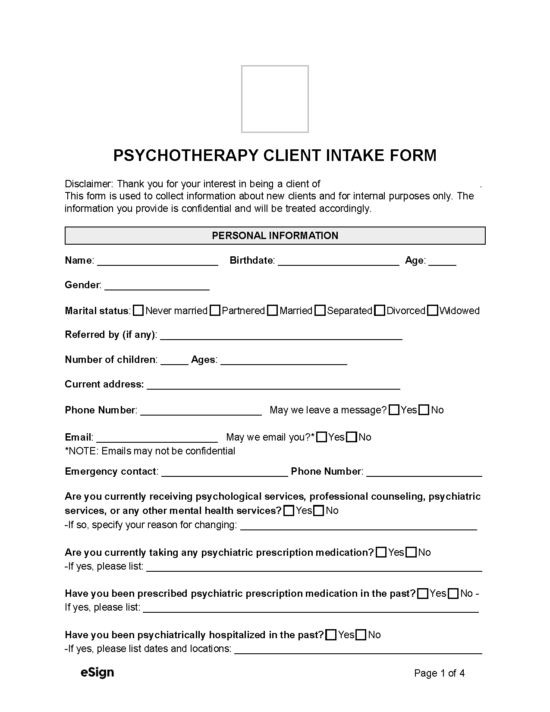
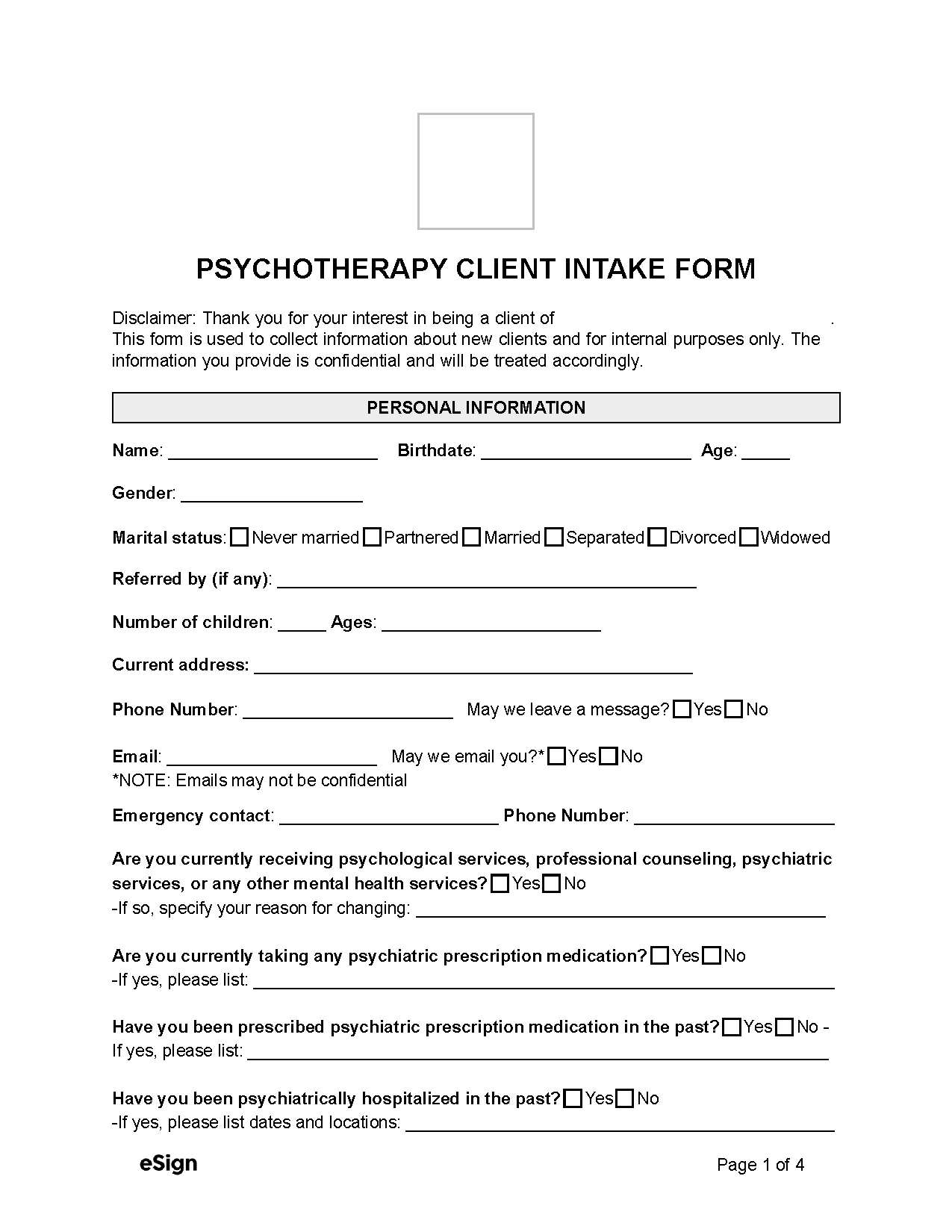
What’s Included
- Personal information – The client’s details, contact information, and treatment history.
- General health information – The client’s current physical health, sleep, lifestyle, and alcohol or substance use.
- Symptoms – The mental health issues requiring treatment.
- Family mental health history – Information on previous mental health diagnoses in the client’s family.
- Personal details – The client’s strengths, coping strategies, and therapy goals.
- Acknowledgment -The client’s signature, and if applicable, that of their guardian.
Protected Health Information (PHI)
The HIPAA (Health Insurance Portability and Accountability Act) protects a client or patient’s information during intake and treatment.[1] Certain exceptions apply, such as:
- If the patient consents to their information being shared.
- If the information is required for payments, treatments, and healthcare operations.
- If it is necessary for preventing harm to the patient or others.
- If disclosing the information is required to comply with a legal investigation.
Furthermore, the SAMHSA’s (Substance Abuse and Mental Health Services Administration) confidentiality regulations provide additional protections for a patient’s substance abuse records and treatment.[2]